OUR FOCUS: Type 1 diabetes
Every day, more than 1.6 million Americans grapple with type 1 diabetes (T1D), a relentless condition that demands constant blood glucose monitoring and insulin therapy for life.1 People living with T1D must adhere to daily stringent lifestyle restrictions that require meticulous planning around every meal, activity, and moment of rest. The emotional toll is profound. People who are affected by T1D often describe living in a state of constant uncertainty and fear around life-threatening complications.
T1D: an autoimmune disorder that hijacks the pancreas and upends lives
What is T1D?
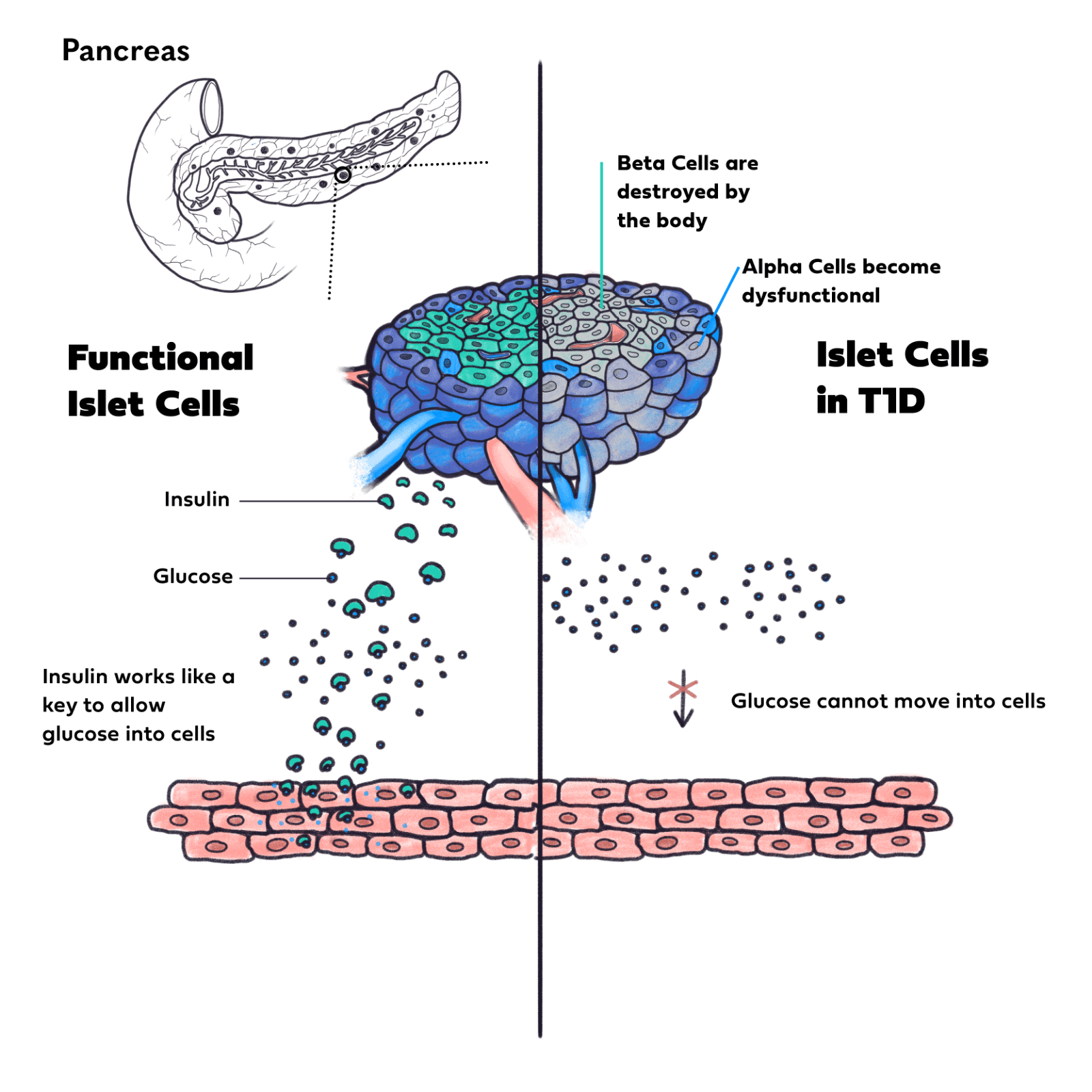
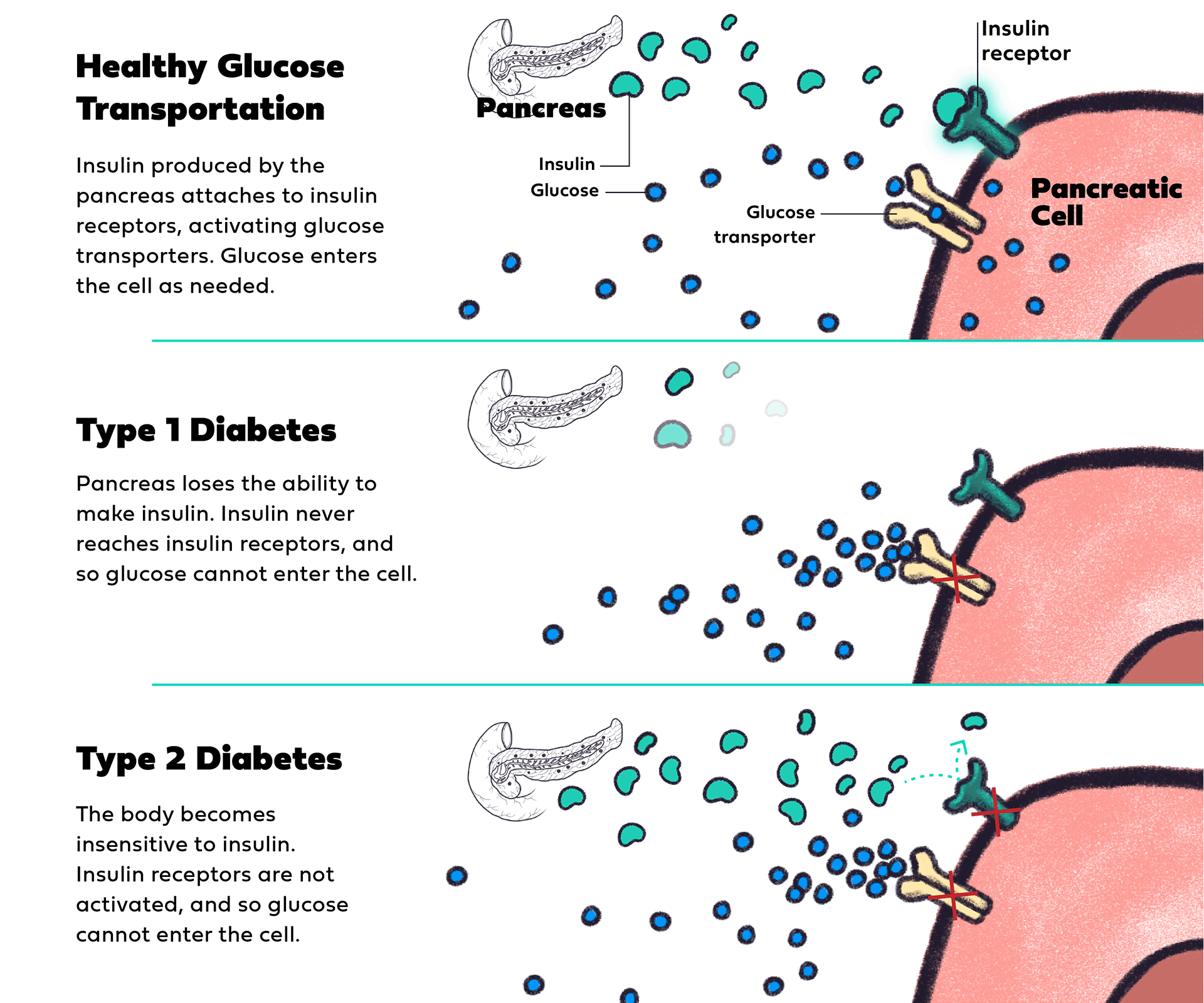
In people without T1D, the body’s blood glucose levels are controlled by clusters of hormone-producing cells in the pancreas known as islets.2 When a person ingests calories from food or drink, their blood glucose level rises. In response, islets in the pancreas release insulin, which acts like a key that opens the door for glucose in the blood to enter cells to be used for energy, enabling blood glucose to baseline.2
However, in people with T1D, the immune system mistakenly attacks and destroys beta cells (insulin-producing cells) in the pancreas.2 As a result, insulin production is impaired or stopped outright, preventing the appropriate uptake of glucose into cells and causing blood glucose levels to rise to dangerously high levels.2 This leads to dysfunction in the pancreatic alpha and delta cells, which produce glucagon and somatostatin, respectively, hormones that each play a key role in blood glucose control.2
As a result, people with T1D lose the ability to regulate blood glucose and can no longer manage how well their body responds to insulin when injected.3 This can lead to potentially life-threatening complications like hypoglycemia.3
How insulin, glucagon, and somatostatin work to regulate blood glucose
Insulin: lowers blood glucose levels by helping glucose enter cells. The pancreas produces insulin in beta cells.
Glucagon: raises blood glucose levels by breaking down glycogen into glucose in the liver. The pancreas releases glucagon when blood sugar levels drop. The pancreas produces glucagon in alpha cells.
Somatostatin: balances insulin and glucagon by suppressing the release of both hormones. The pancreas produces somatostatin in delta cells.2-4
Up to 38% of adults over the age of 30 with T1D may be misdiagnosed with type 2 diabetes (T2D)5
How is T1D different from T2D?
Though most people are familiar with T2D, many know very little about T1D. In the case of T2D, a person gradually develops an insensitivity to the insulin produced by their pancreas over time.6 However, for people with T1D, their pancreas loses the ability to produce insulin due to beta-cell destruction by the immune system.6
T1D
- Pancreas loses the ability to make insulin
Caused by an attack on the immune system
Typically starts in childhood (but can develop at any age)
Symptoms come on quickly
Treated with insulin via injection, insulin pump, insulin pen, or inhaled insulin
Incurable, life-long condition
T2D
- Body becomes insensitive to insulin
- Caused by a combination of lifestyle and genetic factors
- Typically begins in middle age
- Symptoms develop slowly
- Managed with medication, lifestyle changes, and/or insulin
- Potentially reversible in early stages2-6
The history of T1D: from animal-derived insulin to regenerative medicine
- 1899: First scientific understanding of the mechanism of T1D
- 1922: First isolation of insulin
- 1923: Animal-derived insulin preparations are developed
- 1950: Lente insulin is developed
- 1977: Recombinant human insulin is developed
- 2000s: Basal insulin analogues are developed
- 2000s: Sernova’s bio-hybrid organ is developed
Transforming the future of T1D
Leveraging our innovative, implantable biohybrid organ, we can replace the hormones that the body needs to regulate blood glucose levels so that patients with T1D can focus on what matters: living their lives.
REFERENCES: 1. Centers for Disease Control and Prevention. National Diabetes Statistics Report. May 14, 2024. Accessed November 8, 2024. https://www.cdc.gov/diabetes/php/data-research/index.html 2. Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38(10):1964-1974. doi:10.2337/dc15-1419 3. Yosten GLC. Alpha cell dysfunction in type 1 diabetes. Peptides. 2018:100:54-60. doi:10.1016/j.peptides.2017.12.001 4. Rutter GA. Regulating glucagon secretion: somatostatin in the spotlight. Diabetes. 2009;58(2):299-301. doi:10.2337/db08-1534 5. Bao YK, Ma J, Ganesan VC, McGill JB. Mistaken identity: missed diagnosis of type 1 diabetes in an older adult. Med Res Arch. 2019;7(8):1962. 6. Krause M, De Vito G. Type 1 and type 2 diabetes mellitus: commonalities, differences and the Importance of exercise and nutrition. Nutrients. 2023;15(19):4279. doi:10.3390/nu15194279 7. Levy D. History, epidemiology, and aetiology. In: Levy D, ed. Type 1 Diabetes. 2nd ed. Oxford University Press; 2016. Accessed November 1, 2024. https://doi.org/10.1093/med/9780198766452.003.0001